The incidence, severity, morbidity, and mortality of odontogenic infections have declined dramatically over the past 60 years. In 1940, Ashbel Williams published a series of 31 cases of Ludwig’s angina in which 54% of the subjects died. Only 3 years later, he and Dr. Walter Guralnick published the first prospective case in series in the field of head and neck infections, and which the mortality rate of Ludwig’s angina was reduced to 10%. This dramatic reduction in mortality from 54 to 10% was not due to the first use penicillin in the treatment of these infections. Rather, Dr. Guralnick applied the principles of the initial establishment of airway security, followed by early and aggressive surgical drainage of all anatomic spaces affected by cellulites and abscess. Since then, with the use of antibiotics and advanced medical supportive care, the mortality of Ludwig’s angina had been further reduced to 4%. Dentistry has made great progress in prevention and early intervention of odontogenic infection.
Oral and maxillofacial surgeons had made great strides in managing and preventing mortality in severe odontogenic infections. The late Dr. Larry Peterson, who brought the first edition of this text to fruition, articulated the principles of management of odontogenic deep facial space infections. These are eight sequential steps that, if followed with thoroughness and good judgment, will ensure a high level of care for these increasingly uncommon, yet occasionally life-threatening infections.
Thomas R. Flynn, DMD
1.Determine the severity of infection
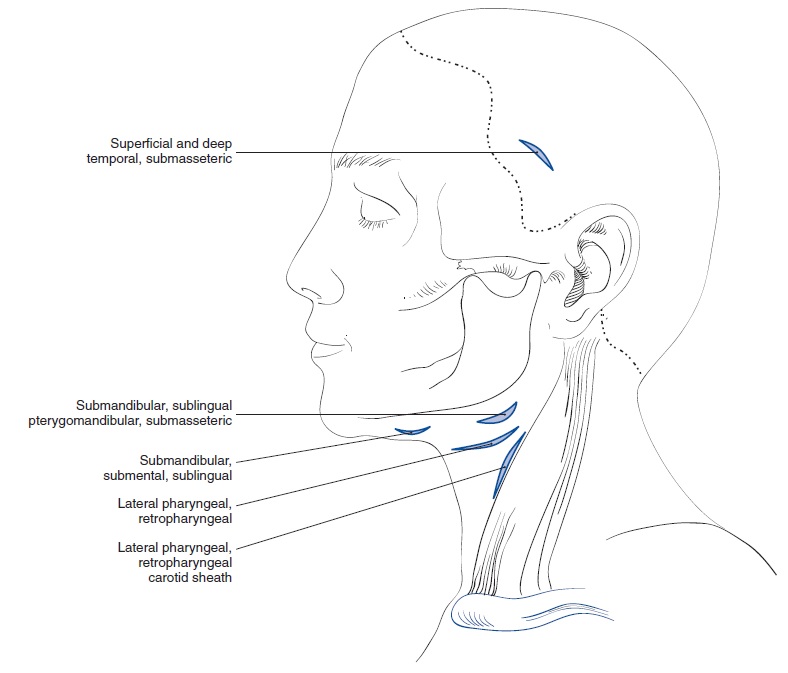
Three major factors must be considered in determining the severity of an infection of the head and neck: anatomic location, rate of progression and airway compromise
2. Evaluate host defenses
Many medical conditions that can interfere with proper function of the immune system, which of course, essential to maintenance of host defense against infection.
- Diabetes
- Steroid therapy
- Organ transplant
- Malignancy
- Chemotherapy
- Chronic renal disease
- Malnutrition
- Alcoholism
- End-stage AIDS (HIV)
The diabetes is listed first because it is the most common immune-compromising disease.
3. Decide on the setting of care
Indicate for hospital admission
- Temperature > 38° C
- Dehydration
- Threat to the airway or vital structures
- Infection in moderate or high severity anatomic spaces
- Need for general anesthesia
- Need for impatient control of systemic disease
4. Treat surgically
It is apparent that immediate establishment (by early intubation or thoracotomy) of airway security and early aggressive surgical therapy are the most important intervention steps in the management of severe odontogenic infections.
5. Support medically
Medical supportive care for the patient with a severe odontogenic infection is composed of hydration, nutrition and control of fever in all patients. Maintenance or reestablishment electrolyte balance and control of systemic disease may also be a crucial part of necessary supportive medical care for some cases.
6. Choose and prescribe antibiotic therapy
The antibiotics choices are separated by severity of infection. Mild or outpatient infections have been shown in a number of studies to respond well to the oral penicillins. There was no significant difference in pain or swelling at 7 days of therapy between penicillin and various others antibiotics, including Clindamycin, Amoxicillin, Amoxicillin-Clavulanate and cephradine. Although these parameters improve more rapidly during the first 48 hours of therapy with alternative antibiotics.
7. Administer the antibiotic properly
The tissue level of antibiotics determines their effectiveness. Those tissue levels are of course dependent on the antibiotic’s level in serum, through which the antibiotic must pass in order to achieve therapeutic levels in soft tissues, bone, brain, and abscess cavities. Administration of antibiotics by the oral route requires that the drug successfully navigate the vagaries of the highly acidic stomach, the chemical qualities of ingested foods, and the basic intestinal tract. Once an antibiotic is absorbed by the gastric or intestinal mucosa, it may then be subject to firstpass metabolism in the liver and subsequent excretion though the bile. Part of the excreted antibiotic may then be reabsorbed by the intestine, resulting in enterohepatic recirculation. For these reasons orally administered antibiotics achieve much lower serum levels at a slower rate than when they are injected directly into the vascular system intravenously.
8. Evaluate the patient frequently
In outpatient infections that have been treated by tooth extraction and intraoral incision and drainage, the most appropriate initial follow-up appointment is usually at 2 days postoperatively
The application of the eight steps must be thorough and the surgeon’s mind must always remain open to the possibility antibiotic resistance, and previously undiagnosed medically compromising conditions. Although adherence to these principles cannot always guarantee a successful result, it can assure the oral and maxillofacial surgeon that he or she is practicing at the highest standard of care. of treatment failure, an error in initial diagnosis
References: Peterson’s Principles of Oral an Maxillofacial Surgery – Chapter 15


Muito bom trabalho meu amigo. Continue nos ajudando. Abraços
Obrigado, João.
Continuarei ajudando, com certeza!